Periodontal disease/Periodontitis/Gum disease explained by a Dental Hygienist
Gum disease is also known as periodontal disease or periodontitis. It affects about half of the adult population in the United States.
How does the dentist determine if you have gum disease?
Your dental providers will take x-rays of your teeth to see if you have normal bone levels between your teeth, and perform a procedure called periodontal probing.
What is periodontal probing?
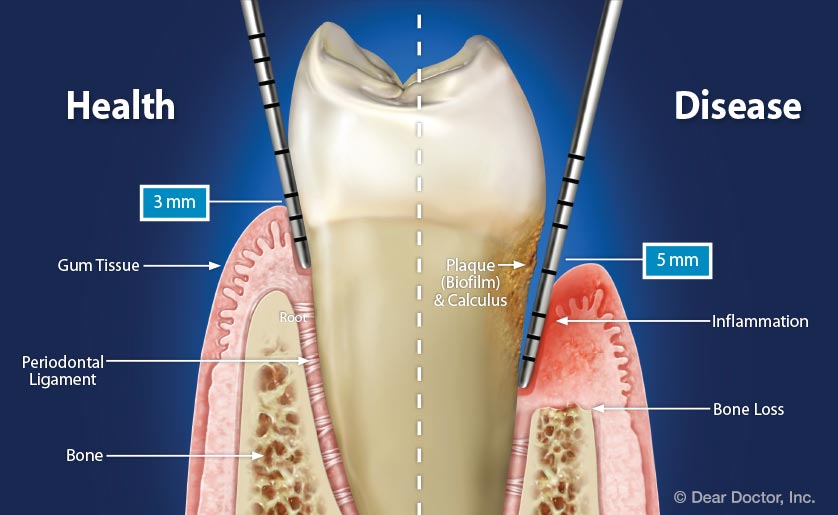
To check the health of your gums, the dentist or dental hygienist will do an examination called periodontal probing to check for “pockets”. When we do that, we’re measuring the spaces between the tooth and the gums with an instrument called a periodontal probe, that is essentially a tiny round ruler. It is not sharp, but sometimes feels a bit pokey, especially if your gums aren’t healthy. If it is too painful, you can ask to have numbing gel put on your gums to make it more comfortable.
What are normal or concerning measurements during periodontal probing?
Normal, healthy gum and bone is hugged up next to the tooth where the enamel meets the root surface. With gum disease, usually from some kind of buildup (from not brushing and flossing, or not getting your teeth cleaned), the gum starts to pull away from the tooth, and you lose the bone that supports your teeth. When you lose bone it doesn’t grow back, so all the damage over your lifetime is cumulative, and if you lose enough bone your teeth get loose and fall out. So, when we take those measurements of the spaces or pockets, 1, 2, & 3 millimeters with no bleeding is normal. This means your gums are healthy.
4 millimeter pockets are borderline, so it can mean you still have healthy bone, just puffy tissue, which is gingivitis. Gingivitis is completely reversible. 4 millimeters could also be the start of bone loss, and 5 millimeters and above are areas where there is bone loss around your teeth, which is more serious gum disease, periodontitis. Periodontitis is not reversible, but it is controllable with proper care at home combined with professional care.
Inflammation from gum disease doesn’t just stay in your mouth, it gets into your bloodstream and contributes to heart disease, diabetes, Alzheimers, colon cancer, worse COVID outcomes, etc. Inflammation in our bodies is always bad.
Great Chart Of Gum Disease
Is recession a sign of gum disease?
Sometimes. Recession, where we can see the root exposed, can happen with healthy or diseased tissue. Recession is a form of bone loss, although it may not have been caused by an active bacterial disease process like periodontitis. It can be the result of gum disease in the past where you lost bone and then the tissue shrank up around the bone, exposing the root. It can also be from other factors like the position of your teeth where they are tipped in, or from orthodontics, where the tooth was moved farther out in bone that may have already been thin, or from abnormal forces on the tooth like clenching and grinding that rock the tooth and cause the bone to fall away, just like if you rocked a post in a pile of dirt. We used to tell patients it was from brushing too hard, which can make it worse, but it usually isn’t the primary cause. If it was just from brushing too hard, it would be even across all of your teeth, not just in some areas, with one tooth having a lot of recession with a tooth next to it not having any.
Are bleeding gums a sign of periodontal disease?
Yes. Bleeding means you have gingivitis or periodontitis. Healthy tissue does not bleed.
What do I need to do to treat gum disease?
To treat mild to moderate periodontal disease, you need a professional procedure called scaling and root planing. You will also need to keep your teeth clean at home with proper brushing and flossing (click here for more tips!), and continue to see your dentist and hygienist for regular maintenance visits. Periodontal disease is not curable, but it is usually controllable.
Professional care for periodontal disease usually starts with a very thorough cleaning of the teeth and root surfaces called scaling and root planing. This is billed to insurance under the codes D4341 and D4342, and is coded per quadrant, so you may have up to 4 separate codes billed. When you have buildup under the gum it’s like having a scrape with rocks and dirt stuck in it. It harbors bacteria and gets infected, so we need to get that all out. You will most likely want to have your gums numbed to some degree so this can be done comfortably. The hygienist or dentist will probably use a combination of ultrasonic scalers and traditional dental scalers to remove the buildup. Treatment may be split into multiple appointments.
After we do scaling and root planing, you have to do your part at home keeping everything clean so it can heal, and prevent that buildup from coming back. This means brushing twice daily (preferably with an electric toothbrush) and flossing or using a waterpik daily (whatever you will actually use to get between your teeth). We will recommend seeing you back for a followup periodontal maintenance cleaning in 3 or 4 months. You may need cleanings 3 or 4 times a year for the rest of your life, or we might extend it out to just twice a year if we can get all the pockets to heal to 3-4mm and you’re doing a good job at home. Your toothbrush and floss really aren’t able to get down below 3mm, and we need to monitor everything carefully to be sure you are not losing more bone. If everything stays stable, you hopefully only have to have scaling and root planing once!
If you have advanced periodontal disease, scaling and root planing may not be effective in treating your condition. If you have pockets deeper than 6 to 7mm, your dentist might refer you to a periodontist, which is a dentist that specializes in treating gum disease, who may recommend surgical procedures.
Why can’t I just get a “regular cleaning” that is covered by my insurance?
Regular cleanings are called prophylaxis, which is defined as “an action taken to prevent disease”. This gets billed to insurance under the code D1110. Unfortunately if there are pockets 4mm and higher, or there is buildup that can be seen on x-rays, you are past the point of prevention. A prophylaxis cleaning will not treat the disease in your mouth, and would be substandard care. The buildup is under the gums and isn’t removed during a standard cleaning, and just removing buildup above the gumline can actually actually make the issue worse because tissues can partially heal and trap that infection.
It’s frustrating for patients and dental professionals that insurance doesn’t pay 100% in these situations where getting this taken care of is even more important. Many dental offices will be willing to work out some kind of payment plan for scaling and root planing with you if you ask. If you have more time than money, dental hygiene schools offer scaling and root planing at extremely reduced cost, and alway need patients. You will still get great care, but it will very likely take more, and longer, appointments to get everything finished.
